Molecular Basis of Epilepsy
Our research
The current focus is on progressive myoclonus epilepsies (PMEs). The central focus of the group’s research is on disease mechanisms of EPM1, the most common PME disease, caused by biallelic partial loss-of-function mutations in the CSTB gene.
CSTB-deficient (Cstb-/-) mice and patient-derived induced pluripotent stem cells (iPSC) are being utilized as models.
We previously showed that CSTB has a role in regulation of neuronal survival during oxidative stress. Early microglial activation and neuroinflammation were shown to contribute to neuronal dysfunction and death in Cstb-/- mice. Recently, we showed that CSTB is involved in the epigenetic regulation of mouse brain development through modulation of histone H3 cleavage. Further, we associated CSTB-deficiency to impaired mitochondrial respiration in neural stem cells and synaptosomes.

To evaluate the biological processes contributing to EPM1 disease progression and to identify potential biomarkers in metabolic pathways, we have performed multiomics analyses of transcriptomics, proteomics and metabolomics from postnatal Cstb-/- mouse brain (Malyutina et al., 2026: revised manuscript submitted). The integrated analysis of transcriptome and proteome data revealed an upregulation of pathways related to the innate immune system activation and lysosomal function, whereas mitochondrial oxidative phosphorylation was consistently downregulated, primarily in the cerebellum. In untargeted and targeted metabolome analyses, we detected changes in pathways related to energy metabolism and oxidative stress, with reduced antioxidant capacity. Together, these findings suggest that CSTB deficiency is associated with impaired brain energy metabolism and early metabolic reprogramming.
We are currently validating the omics findings in patient iPSC -derived neuronal cells with the specific objective to identify molecular targets that define metabolic reprogramming, and to perform treatment experiments in vitro based on this hypothesis. Moreover, we aim to identify disease-specific biomarkers to be utilized in preclinical and clinical studies in the future.
We continue to dissect the molecular genetic basis of PMEs through genome-wide sequencing approaches in collaboration with Prof. Sam Berkovic’s group in Melbourne.
Read more
Group Leader
Senior Scientists
Postdoctoral Researcher
Undergraduate Student
Samia Afroje Rafia
Staff
Exploring the Role of Apolipoprotein ε4 in Progressive Myoclonic Epilepsy Type 1.
Gunnar J, Liu Y, Eronen H, Joensuu T, Äikiä M, Hyppönen J, Silvennoinen K, Mervaala E, Hakumäki J, Lehesjoki A-E, Kälviäinen R. Epileptic disorders. 2025.
In depth behavioral phenotyping unravels complex motor disturbances in Cstb-/- mouse, a model for progressive myoclonus epilepsy type 1.
Pollari E, Tegelberg S, Björklund H, Kälviäinen R, Lehesjoki A-E, Haapalinna A. Frontiers in Behavioral Neuroscience. 2023.
Cystatin B-deficiency triggers ectopic histone H3 tail cleavage during neurogenesis.
Daura E, Tegelberg S, Yoshihara M, Jackson C, Simonetti F, Aksentjeff K, Ezer S, Hakala P, Katayama S, Kere J, Lehesjoki A-E, Joensuu T. Neurobiology of Disease. 2021.
Progressive myoclonus epilepsies – residual unsolved cases have marked genetic heterogeneity including genes in the dolichol-dependent protein glycosylation.
Courage C, Oliver KL, Park EJ, Cameron JM, Grabińska KA, Muona M, Canafoglia L, Gambardella A,Said E, Afawi Z, Baykan B, Brandt C, di Bonaventura C, Chew HB, Criscuolo C, Dibbens LM, Castellotti B, Riguzzi P, Labate A,Filla A,Giallonardo AT, Jackson CB, Joensuu T, Damiano JA, Kivity S, Korczyn A, Palotie A, Striano P, Uccellini D, Giuliano L, Andermann E, Scheffer IE, Michelucci R, Bahlo M, Franceschetti S, Sessa WC, Berkovic SF, Lehesjoki A-E. The American Journal of Human Genetics. 2021.
ZNHIT3 is defective in PEHO syndrome, a severe encephalopathy with impaired cerebellar granule cell migration.
Anttonen A-K, Laari A, Kousi M, Yang YJ, Jääskeläinen T, Somer M, Siintola E, Jakkula E, Muona M, Tegelberg S, Lönnqvist T, Pihko H, Valanne L, Paetau A, Hästbacka J, Kopra O, Joensuu T, Katsanis N, Lehtinen MK, Palvimo JJ, Lehesjoki A-E. Brain. 2017.
A recurrent de novo mutation in KCNC1 causes progressive myoclonus epilepsy.
Muona M, Berkovic SF, Dibbens LM, Oliver KL, Maljevic S, Bayly MA, Joensuu T, Canafoglia L, Franceschetti S, Michelucci R, Markkinen S, Heron SE, Hildebrand M, Andermann E, Andermann F, Antonio Gambardella A, Tinuper P, Licchetta L, Scheffer IE, Criscuolo C, Filla A, Ferlazzo E, Ahmad J, Ahmad A, Baykan B, Said E, Topcu M, Riguzzi P, King MD, Ozkara C, Andrade DA, Engelsen BA, Crespel A, Lindenau M, Lohmann E, Saletti V, Massano J, Privitera M, Espay AJ, Kauffmann B, Duchowny M, Møller RS, Straussberg R, Afawi Z, Ben-Zeev B, Samocha KE, Daly MJ, Petrou S, Lerche H, Palotie A, Lehesjoki A-E. Nature Genetics. 2015.
Abnormal microglial activation in the Cstb-/- mouse, a model for progressive myoclonus epilepsy, EPM1.
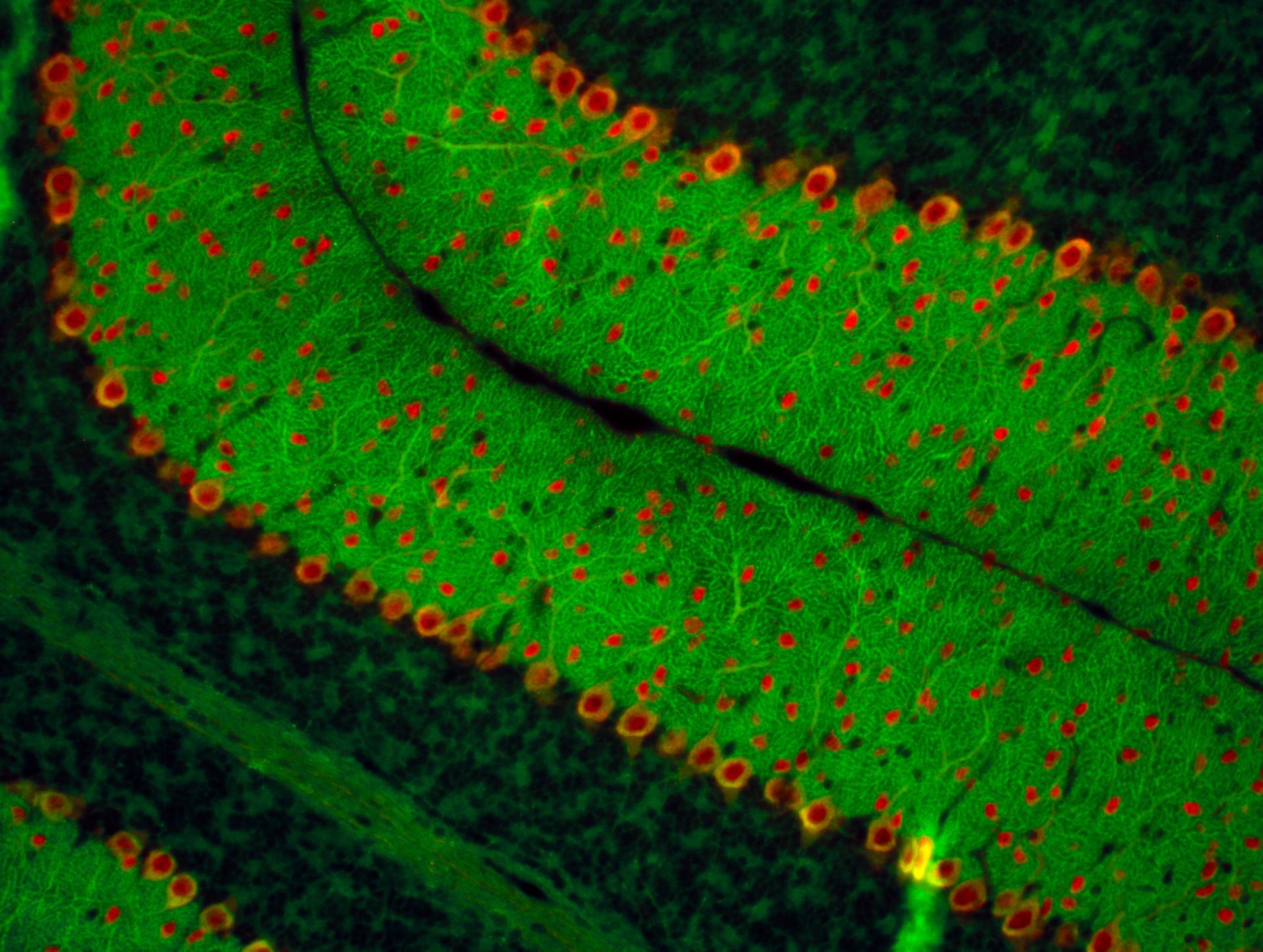
Okuneva O, Körber I, Li Z, Tian L, Joensuu T, Kopra O, Lehesjoki A-E. Glia. 2015.
Early microglial activation precedes neuronal loss in the brain of the Cstb-/- mouse model for progressive myoclonus epilepsy, EPM1.
Tegelberg S, Kopra O, Joensuu T, Cooper JD, Lehesjoki A-E. Journal of Neuropathology & Experimental Neurology. 2012.
Cystatin B deficiency sensitizes neurons to oxidative stress in progressive myoclonus epilepsy, EPM1.
Lehtinen MK, Tegelberg S, Schipper H, Su H, Zukor H, Manninen O, Kopra O, Joensuu T, Hakala P, Bonni A, Lehesjoki A-E. Journal of Neuroscience. 2009.
Mutations in the gene encoding cystatin B cause progressive myoclonus epilepsy (EPM1).
Pennacchio LA, Lehesjoki A-E, Stone NE, Willour VL, Virtaneva K, Miao J, D'Amato E, Ramirez L, Faham M, Koskiniemi M, Warrington J, Norio R, de la Chapelle A, Cox DR, Myers RM. Science. 1996.
Prof. Sam Berkovic, University of Melbourne, Australia
Docent Brendan Battersby, University of Helsinki
Docent Christopher Jackson, University of Helsinki
Prof. Reetta Kälviäinen, University of Eastern Finland
Docent Päivi Saavalainen, Folkhälsan Research Center and University of Helsinki
Folkhälsan Research Foundation
Sigrid Jusélius Foundation
Medicinska understödsföreningen Liv och Hälsa (“Life and Health Medical Fund”)
The Medical Society of Finland (Finska Läkaresällskapet)

